To view the original article, click here.
Hello. I am Dr Tom Chiller, deputy chief of the Mycotic Diseases Branch at the Centers for Disease Control and Prevention (CDC). I am pleased to talk to you about antifungal resistance, a topic that needs more attention.
Although antibiotic-resistant bacterial infections are a widely recognized public health threat, much less is known about the burden and consequences of drug-resistant fungal infections. Since the discovery and widespread use of antibacterial medicines in the 1960s and with increasing numbers of high-risk patients, we have seen the emergence and increased rates of serious invasive fungal infections.
Over the past decade, we have made some progress in combating healthcare-associated bacterial infections. Improving care of central venous catheters and a focus on antibiotic stewardship programs have led to decreases in bloodstream infections caused by resistant bacteria, although we still have a ways to go. However, those decreases have resulted in the fungus Candida becoming the most common cause of healthcare-associated bloodstream infections in many hospitals across the United States.[1] The development of a few classes of antifungal agents has given us the ability to treat these invasive infections, but just like bacteria, some fungi have developed resistance and no longer respond to the antifungals that are used to treat them.
Some types of Candida are becoming increasingly resistant to first-line and second-line antifungals—namely, echinocandins and fluconazole. Approximately 7% of all Candida bloodstream isolates tested at CDC are resistant to fluconazole. Most of these isolates are Candida glabrata, 14% of which are resistant.[2,3] The good news is that CDC’s surveillance data indicate that fluconazole resistance has remained fairly constant over the past 20 years.[3,4,5]
In contrast, echinocandin resistance appears to be on the rise, with 3%-5% of C glabrata isolates being resistant to echinocandin.[2] Isolates tested by CDC before 2004 showed no resistance, so this resistance has emerged after the echinocandins became widely used. Today, the prevalence of echinocandin resistance is more than 10% at some hospitals and is continuing to increase.[6,7]
Finally, a growing concern is the presence of multidrug-resistant Candida infections (those that are resistant to both fluconazole and echinocandins), because few treatment options remain, other than amphotericin B. Not surprisingly, there is growing evidence to suggest that patients who have drug-resistant candidemia have worse outcomes than patients who have susceptible infections.[8,9]
Some studies have indicated that antibacterials may also contribute to antifungal resistance; this could occur for a variety of reasons, one of which is that antibacterials reduce bacteria in the gut and create favorable conditions for Candida growth.[10] It’s not yet known whether decreasing the use of all or certain antimicrobial agents can reduce Candida infections, but appropriate use of antibacterials and antifungals is one of the most important factors in fighting drug resistance.
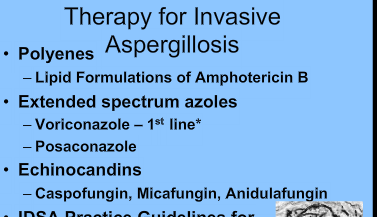
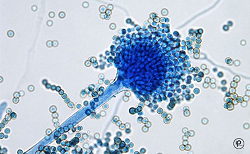
Although most of the resistance that we are concerned about is in Candida species, resistance in other fungi also occurs. I want to highlight the emergence of azole resistance in Aspergillus fumigatus. Since its approval in 2002, the antifungal agent voriconazole has been the primary treatment for invasive aspergillosis. However, more than a decade ago, several countries in Europe began seeing an increasing amount of azole-resistant Aspergillus fumigatus.
Studies in Europe suggest that resistance in Aspergillus may be partially driven by the use of agricultural azoles, which protect crops from fungal diseases.[11,12] Prevalence as high as 30% has been seen in some hospitals in Europe.[13] Patients with these resistant isolates had a much higher mortality—closer to 90%, compared with approximately 40% for patients with susceptible strains.[14] Resistant isolates have been now also identified in the Middle East, Asia, Africa, South America, and most recently in the United States.
The Mycotic Diseases Branch at the CDC is collecting isolates of A fumigatus for US surveillance of resistance. We encourage clinical labs to send samples to CDC. Please refer to the Web resources below for instructions on submitting isolates.
In summary, we encourage hospital executives and infection control staff to:
- Assess antifungal use as part of their antibiotic stewardship programs; and
- Ensure adherence to guidelines for hand hygiene, prevention of catheter-associated infections, and environmental infection control efforts.
We encourage physicians and other hospital staff to:
- Prescribe antifungal medications appropriately;
- Ask their laboratories to routinely determine the species of every Candida sterile body site isolate if it is not reported, and if C glabrata is found, consider ordering antifungal susceptibility testing;
- Document the dose, duration, and indication for every antifungal prescription;
- Be aware of local antifungal resistance patterns; and
- Be active in efforts within your hospital to improve antifungal prescribing.
Medical and Patient education videos
-
Title
Description
-

An interesting description of how a skin prick test is carried out with the intention of finding out which substances a patient is allergic to. Amongst other substances Aspergillus is tested for in this video.
This type of test is quick and easy to carry out and can be useful when screening a large number of allergens. More detailed description
-
The CF Discovery SeriesTM is an informative and engaging program designed to educate and uplift those with cystic fibrosis. Through interactive presentations with experts in the field, those living with cystic fibrosis gain information in a setting which encourages camaraderie and community. You can attend these events in person. Guests attending in person must follow CFRI’s Infection Control Policy, found here.