To view the original Medscape article, click here
Hello. I am Dr. Tom Chiller, a medical epidemiologist at the Centers for Disease Control and Prevention (CDC). Today I am pleased to speak as part of the CDC Expert Video Commentary Series on Medscape.
As you probably are well aware, CDC, in collaboration with state and local health departments and the US Food and Drug Administration (FDA), is investigating a multistate fungal meningitis outbreak among patients who received contaminated steroid injections.
Several patients have suffered from strokes that are believed to have resulted from their infections. This investigation also includes possible fungal infections associated with injections into peripheral joints, such as a knees, shoulders, or ankles.
To date, all identified cases associated with this outbreak have received at least 1 of 3 lots of preservative-free methylprednisolone acetate (MPA) from the New England Compounding Center (NECC).
The fungal infections we are seeing associated with this outbreak are extremely rare. CDC has convened a panel of the nation’s leading clinical fungal experts who are working with us to ensure that our diagnostic and treatment guidance is appropriate for identifying and treating patients who develop infections.
Today I want to give you an update on where we stand with respect to our clinical guidance.
First, here is what we know: To date, more than 300 cases have been reported to us, which includes 24 deaths across 17 states.
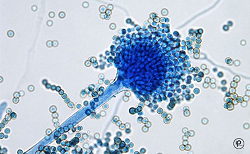
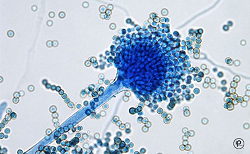
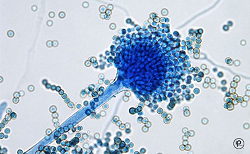
Of cases in which we have identified a fungus, most have been Exserohilum rostratum. One patient has been found to be infected with Aspergillus fumigatus and another with a Cladosporium species. These fungi are common in the environment but were not a recognized cause of meningitis before this outbreak. We are really in new territory when it comes to treatment and management of patients with Exserohilum infection.
CDC and FDA have also confirmed the presence of Exserohilum in 2 of the 3 unopened vials of MPA. We continue to test the third implicated lot of MPA as well as other NECC medications.
Of the approximately 14,000 patients who received injections from 1 of the 3 contaminated lots of MPA, nearly all have been contacted for further follow-up. Among people with meningitis for whom we have clinical information available, the onset of symptoms is typically 1-4 weeks following injection. However, we know that fungal infections can be slow to develop and that there are reports of longer periods of time between injection and onset of symptoms, so we need to monitor these patients for development of signs and symptoms for several months following the injection.
For patients who received epidural or paraspinal steroid injections with medication from any of the 3 recalled lots of MPA, we need to carefully clinically evaluate them. If they have any symptoms consistent with meningitis or posterior circulation stroke, cerebrospinal fluid (CSF) should be obtained for diagnosis unless contraindicated. We also encourage physicians to have a low threshold to obtain CSF in patients with mild signs and symptoms of meningitis because we are aware that some patients in this outbreak have presented with minimal symptoms. When obtaining CSF for diagnosis, we encourage that this be done at a site other than the site used for the steroid injection when possible.
At this time, CDC does not recommend initiation of antifungal treatment in people who received a contaminated steroid injection but who do not have any symptoms or in whom there is no laboratory evidence of infection. However, some patients may be at greater risk than others of developing fungal meningitis. Specific CDC analysis has shown that the greatest risk is in the first 6 weeks after injections.
Clinicians may consider the option of obtaining CSF in patients who received their last injection within the past 6 weeks (42 days) to look for evidence of meningitis before symptoms appear. From our analysis, we have seen that the more time that has passed since the date of the steroid injection, the lower the risk of developing disease.
For patients who are presenting with joint infections, clinicians should collect synovial fluid and/or synovial tissue, either by arthrocentesis or biopsy, and look for evidence of infection.
Let’s shift gears and talk about treatment. If you have a patient who has evidence of fungal meningitis or joint infection, make sure you are following CDC’s treatment recommendations.
At this time, CDC is recommending voriconazole, which is an effective agent for treating infections due to brown-black molds, such as Exserohilum, as well as infections due to Aspergillus species, and has good penetration into the central nervous system.
CDC continues to consult with national experts about treatment options for infections associated with this outbreak. As more information becomes available on patient management, we will continue to update the clinical community.
Please see the links below to stay up to date on the latest CDC guidance.
Finally, because this is an ongoing investigation, we continue to need your help. If you see patients with any suspected adverse events following use of NECC products, please report this to your state health department and FDA’s MedWatch program at 1-800-332-1088 or FDA.gov/medwatch.
Thank you.
Medical and Patient education videos
-
Title
Description
-
Prof. Neil Gow, University of Aberdeen, Fungal update 2015, 10th Anniversary
-
Dr. Elaine Bignell, University of Manchester, Fungal Update 2015, 10th Anniversary
-
Prof. Rob Miller, University College London, Funagl Update 2015, 10th Anniversary
-
Prof. Tom Harrison, St George’s University Hospitals, London, Fungal Update 2015, 10th Anniversary
-
Chair: Prof. Peter Donnelly
Proposers: Drs. Keith Wilson (BMT Unit, Cardiff) & Vanya Gant (Microbiology, UCLH, London)
Opposers: Drs. Brian Jones (Microbiology, Glasgow) & Stephen Ellis (Imaging, Barts, London)Debate – Fungal Update 2015, 10th Anniversary
-
Dr. Jonathan Lambourne, Hospital for Tropical Diseases, London, Fungal Update 2015, 10th Anniversary
Dr. Subathira Dakshina, Genito-Urinary Medicine & HIV, Bart’s Health NHS Trust, London, Fungal Update 2015, 10th Anniversary
-
Prof. Maiken Arendrup, Statens Serum Institut, Denmark, Funal Update 2015, 10th Anniversary
-
Prof Chris Kibbler, University College London, Fungal Update 2015, 10th Anniversary
-
Dr. Frank van de Veerdonk, Nijmegen, The Netherlands
