Submitted by GAtherton on 22 February 2016

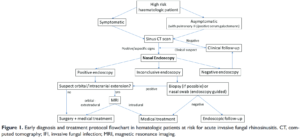
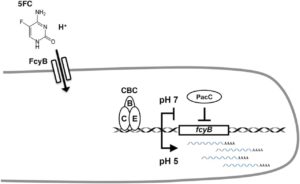
Liver transplants are a well-established life-saving procedure for patients with end-stage liver disease and acute liver failure. However, due to immunosuppression, which is required to lower the risk of organ rejection, patients are particularly predisposed to bacterial and fungal infections. Invasive aspergillosis (IA) is one such infection and can be a significant and serious complication after transplantation. Primary treatments once IA is confirmed include antifungal drugs such as Vfend (Voriconazole). But what if treatment could prevent infection before it even occurs?
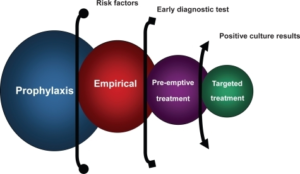
Antifungal prophylaxis (prevention) with voriconazole is known for its efficiency in the prevention of IA. Julius Balogh and colleagues (article) therefore investigated whether prophylaxis with voriconazole could be a successful and cost-effective strategy to reduce the occurrence of invasive aspergillosis infection in high-risk patients after liver transplant.
The authors analysed 339 deceased donor liver transplant recipients between 2008 and 2014 in order to determine whether voriconazole had a preventative effect on the incidence of invasive aspergillosis infection in high-risk liver transplant recipients.
174 patients were considered high-risk recipients and were administered antifungal prophylaxis with voriconazole. Invasive aspergillosis infection was not observed in any of the patients who received voriconazole prophylaxis. The authors concluded that voriconazole prophylaxis is safe, clinically effective and cost-effective in high-risk liver transplant recipients.
News archives
-
Title
Date





 ,
,