Submitted by GAtherton on 23 February 2016
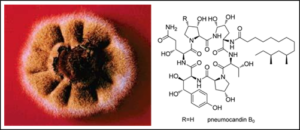
The largely overlooked resident fungal community plays a critical role in human health and disease.
Mahmoud Ghannoum is director of the Center for Medical Mycology at Case Western Reserve University and University Hospitals Case Medical Center and a tenured professor in the Department of Dermatology at the Case School of Medicine in Cleveland, Ohio. Earlier this month he wrote the following article on the lack of research being carried out into the fungal element of our microbiome – i.e. the study of all of the microbes that inhabit our bodies – usually completely harmlessly. Needless to say Aspergillus is found in all parts of our bodies causing no illness.
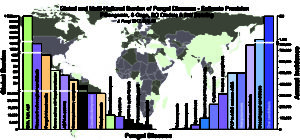
At a workshop held at the National Institutes of Health (NIH) last September on the role of human microbiota in infectious disease, I was disheartened not to hear a single talk on the fungal community—the mycobiome. Disheartened, but not surprised. Ignoring the fungal kingdom is nothing new. More than five years ago, my colleague and I tried to draw attention to this issue in a letter published in Microbe, recommending that the Human Microbiome Project should investigate not just people’s bacterial inhabitants, but the fungal and viral commensal communities as well. While research on the human virome has increased in recent years, the scientific community has not heeded our advice with regard to the fungal components of the microbiome. As of November 2015, only 269 of more than 6,000 Web of Science search results for the term “microbiome” even mention “fungus,” and the scientific search engine returns only 55 papers pertaining to the “mycobiome.”
Despite this lack of attention, a handful of recent studies point to the importance of our commensal fungal inhabitants as critical players in human health and disease. The oral mycobiome of HIV-infected patients differs from that of uninfected controls, for example. Abundance of Candida and Saccharomyces species correlates with increased severity of hepatitis B infections. And an overabundance of the gut fungal pathogen Candida tropicalis aggravates inflammatory bowel disease. As widespread surveys of the mycobiome become available, such correlational data can be further explored by experimental manipulations in the lab. One day, perhaps, researchers will include fungal species in fecal transplants to treat infections by Clostridium difficile and other bacteria, and companies will begin to market probiotic products that contain live cultures of friendly fungi.
News archives
-
Title
Date