Submitted by BethBradshaw on 25 May 2018
In a special issue of Science entitled ‘The Rise of Resistance’, international experts discuss the problem of, and possible solutions to, the antimicrobial resistance timebomb. These open-access articles raise the profile of one of the most urgent challenges to world health.
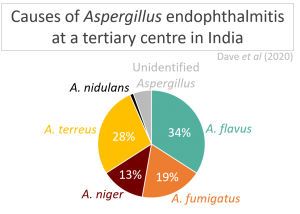
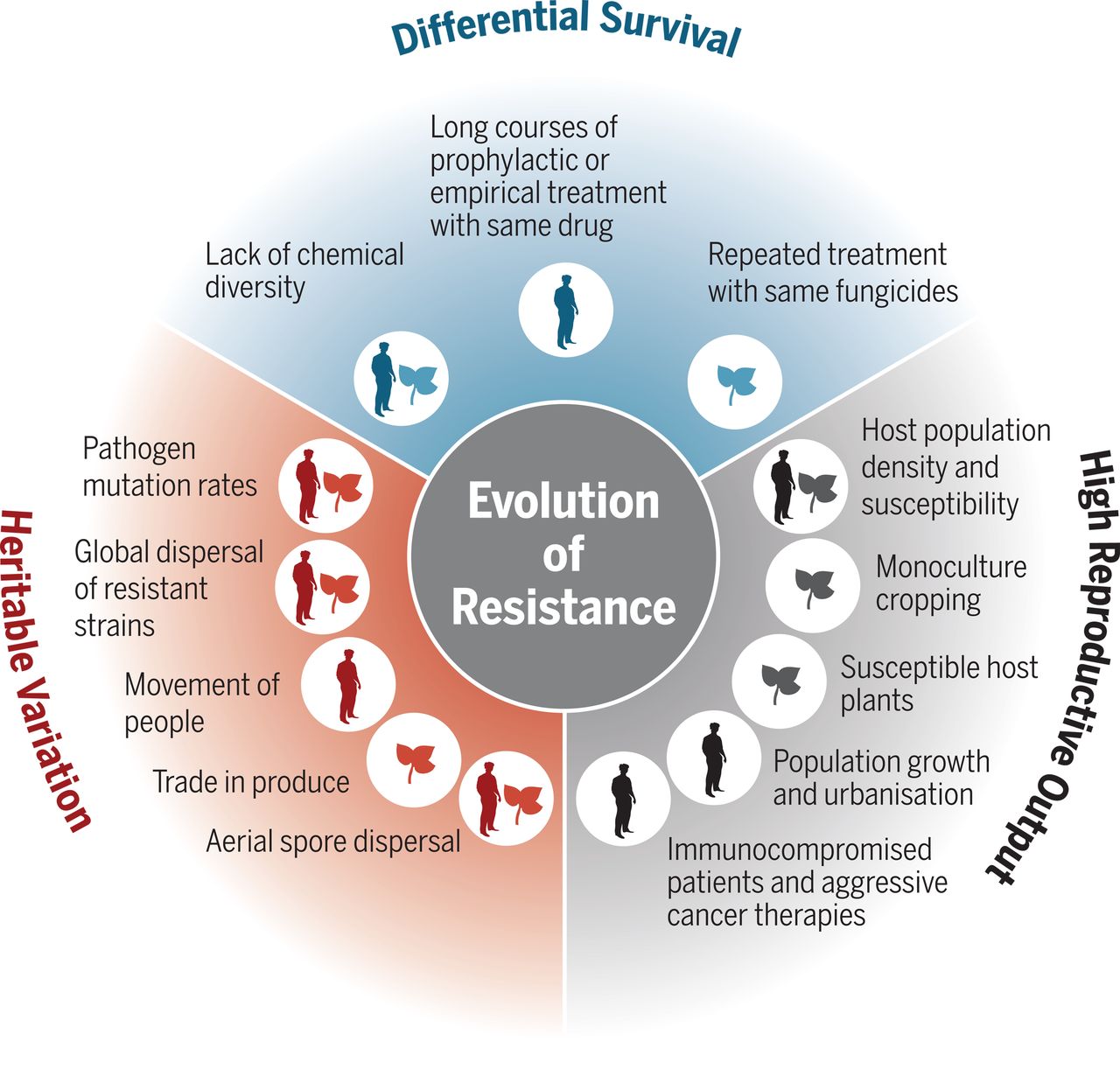
Antifungal resistance can arise through mutations that change the structure/function of quantity of the fungal target protein, or if the fungus gains the ability to pump the antifungal out of its cells. ‘Hypermutator’ strains of Candida glabrata and Cryptococcus neoformans have been seen that evolve especially rapidly because their cellular machinery allows more frequent genetic mutations. Some filamentous fungi are naturally resistant to certain antifungals, and cases caused by these are increasing.
This is mirrored in the global agricultural industry: around 30% of crop yields are lost each year to fungal contamination. While there are many more antifungals available for agricultural uses than clinical uses, the most popular are the azoles (>26% of total fungicide use in the EU), which has been shown to produce resistant strains that can infect humans.
One of the most worrying developments in recent years has been the appearance of Candida auris in 2009, which is resistant to all clinical antifungals and can survive normal hospital decontamination protocols. Another notable example is Aspergillus fumigatus, which can undergo genetic recombination to bring together different combinations of resistance genes.
Unfortunately antifungal resistance is often excluded from schemes to tackle antibiotic resistance. The authors in this issue suggested the following factors as particularly crucial for improving the situation:
· Development of new antifungals. At least 11 antifungals are currently in clinical trials but development is slow and expensive, meaning that multinational pharmaceutical companies are often reluctant to invest.
· Stewardship of existing compounds. Using combinations or lower doses of antifungals can slow the evolution of resistance, and improvements in availability of diagnostics will allow more effective targeting of therapies and more accurate monitoring.
· Integrated disease management. Better practices have been developed for breeding disease-resistant crop plants, which will hopefully reduce the amount of antifungals needed. In humans, disease management would involve reducing the number of at-risk patients through wider availability of antiretroviral therapy for HIV/AIDS patients and development of vaccines against fungal diseases. Immunotherapy may offer another alternative.
Read the Science special issue, including a special paper on antifungal resistance.
Read an accompanying BBC News article.
News archives
-
Title
Date