Submitted by Aspergillus Administrator on 19 November 2010
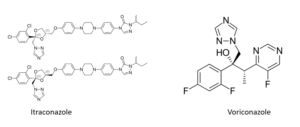
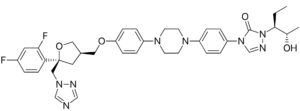
Many of the new drugs used to treat aspergillosis are extremely expensive to use. A course of Voriconazole to treat a chronic infection for example could cost £30 000 per year. Naturally this causes significant problems for the funding bodies and a decision must be made on whether the cost is affordable and justifiable.
There are several factors taken in for account prior to this decision being made, but one of the basic decisions that have to be arrived at is whether the cost is justified for a given group of patients as judged by questions on how much improvement they will see in their general condition, symptoms, longevity or quality of life. An important part of the answer to some of these questions are published research that demonstrates the effectiveness of a drug for that group of patients.
Once all the information that can be collected to support a particular drug application has been gathered it has to be sent to the organisation required to make the funding decision. In the UK that responsibility belonged to the National Institute for Clinical Excellence (NICE). This single body was able to pass binding resolutions that banned the purchase of any drugs using NHS funds that it found to be too expensive to use considering the benefit it brought a particular group of patients. As you might imagine many battles were fought by patients groups against NICE each time new evidence of efficacy of a new drug came to light, and the decisions of NICE were often controversial.
Decisions often took years to arrive and now health budgets are falling all round the world it is likely that more controversy will follow. Despite this NICE is used as a model system around the world to control spending on drugs.
The UK government is now proposing to take the power to ban the use of new drugs away from NICE and give it to local funding bodies run by local general doctors (GP’s in the UK) who they think will be better suited to deciding which patients groups get new drugs. These groups may well be less remote from patients but they will be bound by the same shortage of money that NICE had to deal with – in fact probably worse! At least patients groups can now appeal to authorities closer to home and some may get funding rather than there being a single blanket ban.
NICE had yet to produce guidelines for the use of antifungals in respiratory infections, or at least I cannot find any on their website. They will apparently continue to work on those documents.
So how are antifungal funded for respiratory infections in the UK? The decisions are already made at a local level, currently by the Primary Care Trust. Funding is allowed in the NHS until such time as NICE guidelines say otherwise – and of course now NICE guidelines will not have the power to ban the use of antifungals for this purpose – perhaps that is good news for some patients as the status quo may continue but not for those patients already waiting for funding as they have had funding refused by their local PCT.
News archives
-
Title
Date






![Gulu referral hospital[2] Gulu referral hospital[2]](https://www.aspergillus.org.uk/wp-content/uploads/2019/03/Gulu-referral-hospital2_0-232x300.png)