Submitted by HLeSueur on 27 May 2016
 Previous studies of antifungal therapy in patients with asthma and chronic sinusitis have produced mixed results. Despite a wealth of data supporting their use (e.g. Denning et al. 2009), some attempts to use antifungal rinses have failed to produce an effect. Daniel Hamilos, from Harvard Medical School says this is likely due to poor selection of patients.
Previous studies of antifungal therapy in patients with asthma and chronic sinusitis have produced mixed results. Despite a wealth of data supporting their use (e.g. Denning et al. 2009), some attempts to use antifungal rinses have failed to produce an effect. Daniel Hamilos, from Harvard Medical School says this is likely due to poor selection of patients.
Dr Evan Li and colleagues, from the Baylor College of Medicine in Houston conducted a retrospective analysis in 134 patients, who had all been referred to an allergy clinic in Houston due to uncontrolled asthma. All patients provided sputum samples that were tested for fungi. Dr Li explained that the method of fungal culture is critical and that existing methods are unreliable. Sputum contains immune cells and antifungal compounds, which can impede growth in culture, leading to poor selection of patients suitable for antifungal therapy. Li used a more reliable method of fungal culture, treating sputum samples with dithiothreitol (300mg/mL of sputum) samples were then vortexed and centrifuged until pellets were produced. The pellets were then re-suspended and applied to growth plates. The second step increased the sensitivity of the culture, providing near 100% specificity and sensitivity, allowing for the careful selection of patients.
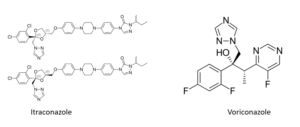
Of the 134 patients tested, 112 (83.5%) had a positive culture (defined as the formation of at least six colonies in 4 weeks. 75 were subsequently treated with voriconazole, terbinafine, fluconazole, or a combination. In 90% of those treated with voriconazole, there was significant improvement in symptoms. Benefits included less sputum production, improved breathing, less coughing and less rescue inhaler use.
The next step is to conduct a prospective clinical trial, and the researchers hope to prove that antifungals are a very effective treatment for asthma and chronic sinusitis.
News archives
-
Title
Date





![Gulu referral hospital[2] Gulu referral hospital[2]](https://www.aspergillus.org.uk/wp-content/uploads/2019/03/Gulu-referral-hospital2_0-232x300.png)