Allergic Bronchopulmonary Aspergillosis (ABPA) is a condition which produces an allergy to the spores of the Aspergillus moulds. It is quite common in asthmatics; up to 2.5% of adult asthmatics might experience this at some point throughout their lives. ABPA is also common in cystic fibrosis patients as they reach adolescence and adulthood (around 5-10% CF patients may be affected).
Presentation:
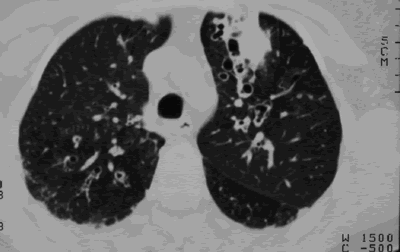
The symptoms of ABPA are similar to those of asthma: intermittent episodes of feeling unwell, coughing and wheezing. Some patients cough up brown-coloured plugs of mucus. There may be pulmonary infiltrates, which do not respond to conventional antibiotics. A diagnosis can be made by X-ray or by sputum, skin and blood tests. An elevated total serum IgE, together with evidence of Aspergillus sensitisation as seen by either the presence of Aspergillus antibodies, or identification from respiratory fluid, is a positive indication. In the long term, ABPA can lead to permanent lung damage (fibrosis or bronchiectasis) if untreated.
Treatment:
The treatment for ABPA is steroids taken by aerosol or mouth (prednisolone), especially during attacks. Itraconazole (an oral antifungal drug) is useful in reducing the amount of steroids required in those needing medium or high doses. This is beneficial as steroids have side-effects like thinning of the bones (osteoporosis) and skin, as well as weight gain (especially when used for a long time). It is not known whether patients with ABPA who are not taking steroids (or are on low doses) benefit from antifungals.